PRN Medication Use is one of the few sections of the revised F605 (Right to Be Free From Chemical Restraints/Unnecessary Psychotropic Medications) in Appendix PP of the State Operations Manual that does not have changes that went into effect on April 28, 2025. However, the updated examples of F605 noncompliance include a greater emphasis on PRN (as needed) use of antipsychotic medications and other psychotropic medications (i.e., anti-depressant, anti-anxiety, and hypnotic medications).
There is not only a revised, more detailed example of a Level 4 (Immediate Jeopardy (IJ) to Resident Health and Safety) citation, there are also new examples of Level 3 (Actual Harm That Is Not Immediate Jeopardy) and Level 2 (No Actual Harm With Potential for More Than Minimal Harm That Is Not Immediate Jeopardy) citations, as shown in the following excerpt from Appendix PP:
| F605 Examples of Noncompliance Involving PRN Antipsychotic/Psychotropic Medications Examples of Level 4 (Immediate Jeopardy to Resident Health and Safety) include, but are not limited to: A PRN antipsychotic medication initiated more than 14 days ago, originally prescribed for acute delirium, continued to be administered daily without re-evaluation, and with no evidence of monitoring for adverse consequences. The failures to monitor for adverse consequences and re-evaluate the appropriateness of giving the medication created a likelihood for serious harm from adverse consequences and a significant decline in functioning. Examples of Level 3 (Actual Harm That Is Not Immediate Jeopardy) include, but are not limited to: A resident has an order for a PRN psychotropic medication that the resident can take for anxiety. However, staff regularly administer the PRN psychotropic medication to the resident with no documented indication but during an interview, staff explained the medication helps the resident sleep, so they’ve been giving it nightly even though the resident did not request it. Since receiving the medication, the resident has been sleeping through breakfast and has experienced significant weight loss. Examples of Level 2 (No Actual Harm With Potential for More Than Minimal Harm That Is Not Immediate Jeopardy) include but are not limited to: A resident was prescribed a PRN psychotropic medication for episodes of anxiety which can have a sedating effect. The resident is no longer experiencing anxiety and has not requested the medication for over a week. Although the medication has not been administered recently, the PRN order has been in place for more than 14 days, and there is no documented rationale for extending the order for the medication. |
Note: The chart “PRN Psychotropic Medications in the Unnecessary Medications, Chemical Restraints/Psychotropic Medications, and Medication Regimen Review Critical Element Pathway Combined With the F605 Guidance” at the end of this article explains the process that surveyors will use to assess compliance with the regulations covering PRN psychotropic medications.
PRN psychotropic medication use is high risk, says Amy Lee, RN, BSN, MSN, CRRN, QCP, president and CEO of Coretactics Healthcare Consulting in Rexford, NY. “Generally, you should work with the medical director to encourage prescribers to limit PRNs across the board with these four drug classes.”
The problem with PRN psychotropic medications is inadequate documentation, especially when these medications are prescribed for residents who have acute or intermittent behaviors, says Lee. “Insufficient documentation is a common concern across healthcare. It’s not just a problem in nursing homes. However, you have to implement a process to ensure that you have the documentation in place that supports that specific resident’s need for PRN antipsychotic or other psychotropic medications.
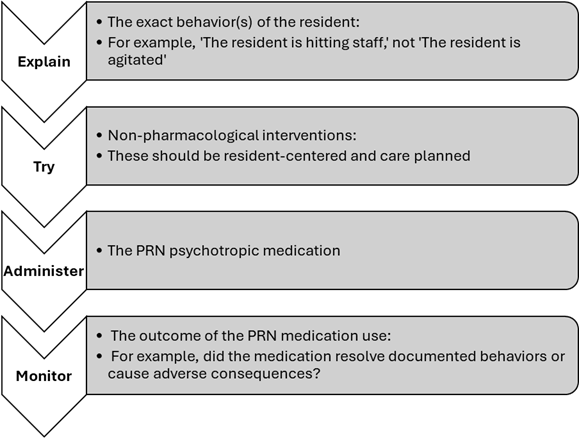
Lee offers the following four steps for the director of nursing services (DNS) and other nurse leaders to teach nursing staff to take when they plan to administer a PRN psychotropic medication to a resident who is experiencing behaviors:
Step 1: Document the behavior
“First, staff need to explain the exact behavior that the resident exhibited prior to administration of the medication,” stresses Lee. “The documentation should not focus solely on how the resident was feeling. You should ask them to avoid making notes that only say, for example, ‘The resident was agitated,’ or ‘The resident was anxious.’”
Instead, staff should document the resident’s actions, recommends Lee. “What action did the resident take to express their emotions? For example, were they hitting, kicking, pinching, screaming, or crying? Whatever the resident was actually doing is what staff need to document.”
Step 2: Document attempted non-pharmacological interventions
Next, staff must document all the non-pharmacological approaches that they tried prior to administering the PRN psychotropic medication, says Lee. “Whatever non-pharmacological interventions are in the care plan to address the diagnosed specific condition that the PRN medication is prescribed for should be attempted and documented.”
For example, did staff try bringing the resident to a quiet area? asks Lee. “Did they try giving them a warm blanket? Did they try soothing music? The documentation needs to show what the staff tried first each time that the PRN medication is given.”
Step 3: Document medication administration
“If none of the resident-centered non-pharmacological interventions were effective, staff then need to administer the PRN psychotropic medication and document it,” says Lee. “Staff need to understand that administering the PRN psychotropic should always come after the attempt at non-pharmacological intervention.”
Step 4: Document the outcome of medication administration
“Between 30 minutes to an hour after staff administer the PRN psychotropic medication, they need to document to answer the question, ‘What was the outcome for the resident?’” says Lee. “Staff should monitor and document the resident’s response to the PRN psychotropic medication. For example, did the PRN medication alleviate the resident’s documented behaviors? Did the resident experience any potentially medication-related adverse consequences?
The following chart sums up Lee’s approach to documenting the use of PRN psychotropic medications:
PRN Psychotropic Medications in the Unnecessary Medications, Chemical Restraints/Psychotropic Medications, and Medication Regimen Review Critical Element Pathway Combined With the F605 Guidance
| Surveyor Interview With Pharmacist ☐ How do you evaluate PRN medications, specifically PRN psychotropic and antipsychotic medications? |
| Surveyor Record Review for F605 ☐ Is there evidence that the limitations for use of PRN psychotropic and antipsychotic medications have been met? F605 guidance on those limitations: ☐ Psychotropic medications may be prescribed on a PRN basis in certain situations, such as: — While the dose is adjusted, — To address acute or intermittent symptoms, or — In an emergency. ☐ Residents must not have PRN orders for psychotropic medications unless: — The medication is necessary to treat a diagnosed specific condition. ☐ For acute or emergency situations where the symptoms have stabilized: — The staff and prescriber should consider whether medications are still relevant. ☐ The attending physician or prescribing practitioner must document: — The diagnosed specific condition and indication for the PRN medication in the medical record. (§483.45(e)(3-5). ☐ The table below explains additional limitations for PRN psychotropic (other than antipsychotic medications) and PRN antipsychotic medications: 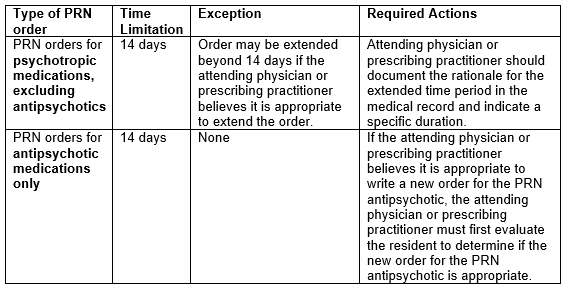 ☐ The required evaluation of a resident before writing a new PRN order for an antipsychotic entails: — The attending physician or prescribing practitioner directly examining the resident and assessing the resident’s current condition and progress to determine if the PRN antipsychotic medication is still needed. — As part of the evaluation, the attending physician or prescribing practitioner should, at a minimum, determine and document the following in the resident’s medical record: • Is the antipsychotic medication still needed on a PRN basis? • What is the benefit of the medication to the resident? • Have the resident’s expressions or indications of distress improved because of the PRN medication? — Report of the resident’s condition from facility staff to the attending physician or prescribing practitioner does not constitute an evaluation. |
| Critical Element Decision 2 Psychotropic Medications, did the facility ensure that: ☐ PRN use is only if necessary to treat a specific, diagnosed, and documented condition; ☐ PRN orders for psychotropic medications which are not for antipsychotic medications are limited to 14 days, unless the attending physician/prescribing practitioner documents a rationale to extend the medication; ☐ PRN orders which are for antipsychotic medications are limited to 14 days, without exception and the attending physician/prescribing practitioner did not renew the order without first evaluating the resident? If No to any of the above, cite F605. |
This AAPACN resource is copyright protected. AAPACN individual members may download or print one copy for use within their facility only. AAPACN facility organizational members have unlimited use only within facilities included in their organizational membership. Violation of AAPACN copyright may result in membership termination and loss of all AAPACN certification credentials. Learn more.

