The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) code assignment continues to be a bit of an enigma in the long-term care setting. Members regularly ask questions about ICD-10-CM coding in AAPACN’s online communities, as well as in post-education surveys, often confused about how to order the codes. The ICD-10-CM coding guidelines are designed to provide coders with the tools they need to assign correct codes, including considerations for code sequencing, particularly etiology and manifestation codes. This article explores key coding guidelines relevant to correct sequencing and application to ICD-10-CM codes.
Etiology and Manifestation Coding
Etiology and manifestation coding requires capturing both the underlying cause (the etiology) and the resulting condition (the manifestation). ICD-10-CM has specific rules for these types of conditions, often seen as a condition “in diseases classified elsewhere.” It offers clear guidance on how to sequence etiology and manifestation codes.
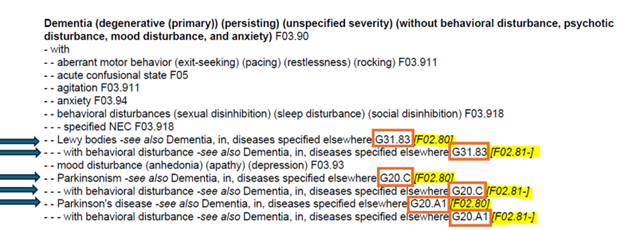
The etiology code must be listed first, followed by the manifestation code. For example, a resident has dementia with Parkinson’s disease. In the Alphabetic Index, a code from category G20 is followed by code F02.80 or F02.81- shown in square brackets. The code from category G20- represents the underlying etiology, Parkinson’s disease, and it must be sequenced first. Codes F02.80 and F02.81- represent the manifestation of dementia in diseases classified elsewhere, with or without behavioral disturbance.
In the Alphabetic Index, the code in brackets (highlighted here in yellow) is always sequenced after the preceding etiology code (shown in orange box) and can never be the primary or admitting diagnosis.
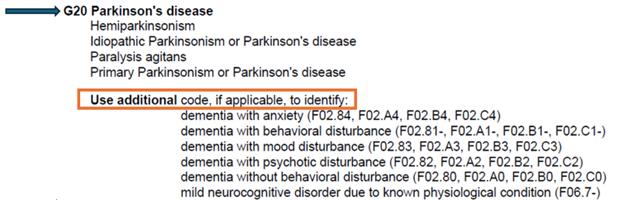
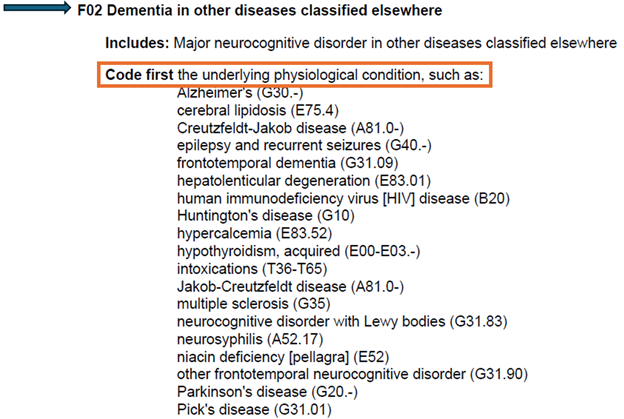
When these codes are then reviewed in the Tabular List, the appropriate method of assigning codes, additional instruction to support this sequence, is provided at the three-digit character code.
Note: When reviewing codes in the Tabular List after looking up a condition in the Alphabetic Index, note the three-digit character code (first three digits of the code) in the Tabular List first for additional guidance before reviewing the full code.
These additional notes may advise “Use additional code,” seen at the etiology code, or “Code first,” identified at the manifestation code.
Using our example of Parkinson’s disease, the Tabular List review starts at G20 (blue arrow). Because Parkinson’s disease is the etiology code, the “Use additional code” instruction instructs use of an additional diagnosis and code from a list. Next the Tabular List confirms the final G20 code as the highest level of specificity available in the physician documentation. The coder would then use the Tabular List to find the appropriate additional code from category F02.
The three-digit character code must be reviewed first to determine if additional coding instruction is available. In the next image, the “Code first” instruction (orange box) is located at F02 (blue arrow).
Here are examples of other manifestation codes “in diseases classified elsewhere” that require another code to be sequenced first:
- (B95-B97) Bacterial and viral agents as the case of diseases classified elsewhere
- (D63) Anemia in chronic diseases classified elsewhere
- (G63) Polyneuropathy in diseases classified elsewhere
- (I68) Cerebrovascular disorders in diseases classified elsewhere
- (J17) Pneumonia in diseases classified elsewhere
For more information on the etiology and manifestation codes, see section I.A.13 of the ICD-10-CM Official Guidelines for Coding and Reporting.
“Code First” and “Use Additional Code” Sequencing
“Code first” and “Use additional code” instructions are not always associated with etiology and manifestation codes. But when used for other types of codes, the sequencing rules still apply. That is, a diagnosis code with an instruction to code another code first cannot be sequenced before that code or be coded as a primary or admitting diagnosis.
For example, codes from the three-digit category code G46 cannot be a primary or admitting diagnosis because the “Code first” instruction explains that “underlying cerebrovascular disease” must be coded first.
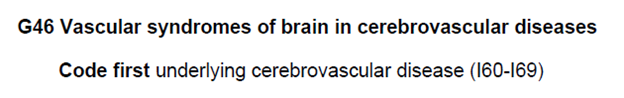
If a diagnosis under the “Code first” instruction is not supported by physician documentation in the medical record, the physician should be queried for clarification for the presence of the code or the accuracy of the original code reviewed that contained the “Code first” instruction. Thus in the example, if the physician documented vascular syndrome but did not specify the cerebrovascular disease, he or she should be queried about the type of cerebrovascular disease.
Note: In the SNF setting, codes from category I69 are typically used to indicate sequela of cerebrovascular disease.
Impact on the Patient-Driven Payment Model
Many return-to-provider diagnoses in the PDPM mapping tool for the primary diagnosis for the clinical category determination relate to the ICD-10-CM coding guidance on etiology/manifestation or “code first” instructions. If another diagnosis should be coded first, these codes would never map to one of the 10 Clinical Categories necessary for case-mix group calculation. Many insurers also use this ICD-10-CM guidance to determine if primary diagnosis codes are inappropriate.
For additional information on sequencing using the “Code first” coding convention, see section I.B.7, Multiple coding for a single condition, in the ICD-10-CM Official Guidelines for Coding and Reporting.
Conclusion
The ICD-10-CM guidelines can help users achieve accurate coding. Understanding the sequencing rules for etiology/manifestation coding will ensure compliance. By following these guidelines, coders can reflect the resident’s conditions accurately and also guarantee that the appropriate sequence is used on the claim. Correct sequencing and adherence to “Code first” and “Use additional code” instructions reduce errors on resident diagnosis coding and promote proper reimbursement.
Additional ICD-10-CM coding information is available in these helpful AAPACN resources:
AAPACN Articles:
- Five Mistakes Often Made Selecting ICD-10-CM Codes in the SNF
- How to Use the ICD-10-CM Coding Manual
- ICD-10-CM: Navigating the Term “With,” Combination Codes, and Complications of Care
- Deep Dive into ICD-10-CM Coding: Misunderstood Coding Guidelines
- ICD-10 Coding: Keys to Achieving the Highest Specificity
- Updates to ICD-10-CM Coding Guidelines: Key Revisions and Their Implications
AAPACN Education:
- ICD-10-CM Coding Certificate Program for SNFs
- RAC-CT – Introduction to ICD-10-CM Coding for Long-Term Care
AAPACN On-Demand Webinar:
AAPACN Podcasts:
- ICD-10 Diagnosis Coding for Skilled Nursing Facilities with Carol Maher
- ICD-10-CM Codes: Use of Unspecified Codes Resulting in Medicare Denials
- Follow-Up Answers to Q&A from ICD-10 Updates Sept. 12, 2024, AAPACN Webinar
AAPACN Tool:
This AAPACN resource is copyright protected. AAPACN individual members may download or print one copy for use within their facility only. AAPACN facility organizational members have unlimited use only within facilities included in their organizational membership. Violation of AAPACN copyright may result in membership termination and loss of all AAPACN certification credentials. Learn more.

